In a groundbreaking study published in the Proceedings of the National Academy of Sciences (PNAS), Japanese researchers from Tokyo Medical and Dental University (TMDU) have made a significant leap in regenerative medicine.
Their work focuses on the promising possibilities of recreating and rebuilding body tissues and organs using stem cells, potentially offering an alternative cure for various diseases.
The researchers’ primary focus was on the parathyroid glands (PTGs), small endocrine glands responsible for maintaining calcium balance in the body by producing the parathyroid hormone (PTH).
Hypoparathyroidism, a condition where PTGs fail to produce enough PTH, can be caused by congenital factors or acquired, most commonly due to neck surgery.
Current treatment methods, including calcium supplements and Vitamin D analogs, often have limitations, necessitating lifelong replacement therapy.
A Breakthrough Experiment: Functional PTGs Generated from Mouse Embryonic Stem Cells
The research team’s aim was to generate functional PTGs from mouse embryonic stem cells (mESCs) as a step towards potential clinical applications in humans.
The challenge lied in creating PTG cells that respond to changes in calcium concentration in vitro.
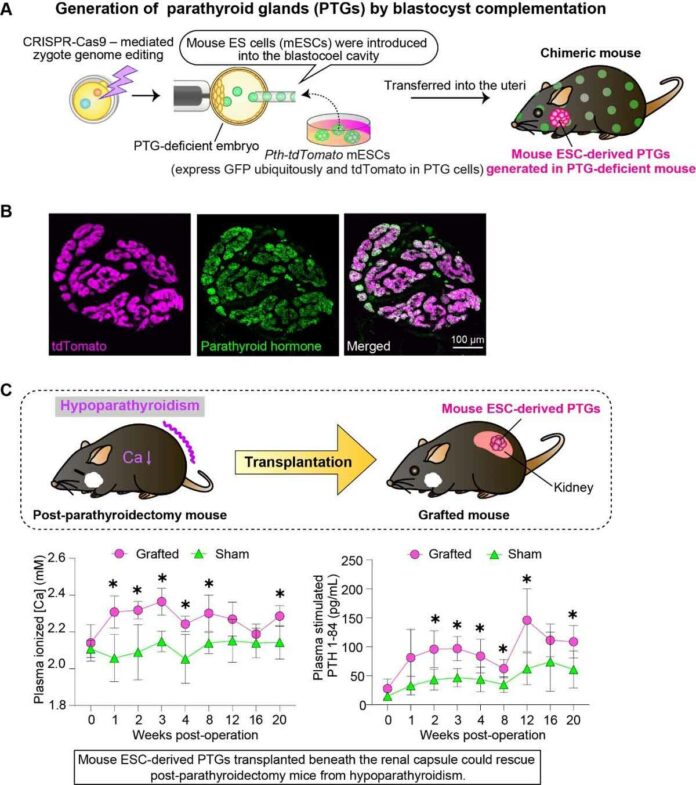
To address this, they employed a method called “blastocyst complementation,” using mouse organisms as their initial test subjects.
Blastocyst Complementation: Paving the Way for Organ Regeneration
Blastocyst complementation involves preparing blastocysts from mutant animals that lack specific organs and then injecting them with pluripotent stem cells.
As a result, the entire organ of the chimeric animal develops from the injected stem cells.
This innovative approach holds the potential to revolutionize organ regeneration in vivo.
Successful Generation of Functional PTGs
To create a PTG-deficient mouse embryo for blastocyst complementation, the researchers utilized CRISPR-Cas9 genome editing.
The injected mESCs differentiated into mature PTGs within the chimeric mouse body, displaying all the necessary functions, including responding to extracellular calcium and regulating PTH secretion.
Furthermore, the transplanted mESC-derived PTGs showed promising results by improving the pathology of a hypoparathyroidism model mouse.
Cross-Species Success: Functional PTGs in Rats
Excitingly, the researchers also demonstrated the effectiveness of their method in cross-species studies.
They successfully produced functional mouse PTGs in rats, further strengthening the potential for clinical applications in the future.
Hope for Endocrine Organ Regeneration
While this breakthrough study was conducted in mice and rats, it sets the stage for further advancements in regenerative medicine and endocrine organ regeneration.
The ability to generate functional PTGs from stem cells could open up new treatment avenues for patients suffering from hypoparathyroidism and other related conditions.
Towards Clinical Applications
The ultimate goal of the research is to translate these findings into clinical applications in humans.
By showcasing successful organ generation in vivo, the study brings hope to patients in need of organ transplants and regenerative therapies.
Future Prospects
The researchers’ pioneering work not only sheds light on the possibilities of regenerative medicine but also highlights the significance of blastocyst complementation as a powerful tool for generating functional organs.
As technology and understanding continue to advance, we can expect even more remarkable breakthroughs in the field of regenerative medicine, offering hope to countless individuals battling various medical conditions.
In conclusion, the research by the Tokyo Medical and Dental University marks a major advancement in the field of regenerative medicine.
Their success in generating functional PTGs from stem cells represents a crucial step towards the future of organ regeneration and transplantation therapies.
As scientists worldwide continue to explore the potential of stem cells and blastocyst complementation, the dream of harnessing regenerative medicine to cure diseases and heal the human body may soon become a reality.
FAQs
Regenerative medicine is a branch of medical science that focuses on harnessing the body’s natural regenerative capabilities to repair, replace, or restore damaged tissues and organs. This field holds immense promise in offering alternative treatments for various diseases and conditions.
Parathyroid glands are small, pea-sized endocrine glands located in the neck, adjacent to the thyroid gland. Their primary function is to produce and secrete parathyroid hormone (PTH), which plays a crucial role in regulating calcium levels in the body.
Hypoparathyroidism is a medical condition where the parathyroid glands produce insufficient amounts of PTH. This leads to imbalances in calcium levels, resulting in symptoms like muscle cramps, tingling sensations, and weakened bones.
The conventional treatment for hypoparathyroidism involves lifelong replacement therapy, including calcium supplements and Vitamin D analogs. In some cases, full-length recombinant human PTH is used. However, these treatments may have limitations and may not fully address the condition’s complexities.
Blastocyst complementation is a novel technique in regenerative medicine where blastocysts (early-stage embryos) from mutant animals lacking specific organs are injected with pluripotent stem cells. The injected stem cells then contribute to the development of the entire organ in the resulting chimeric animal.
In the study by Tokyo Medical and Dental University, researchers used blastocyst complementation to generate parathyroid gland-deficient mouse embryos. They injected mouse embryonic stem cells (mESCs) into the blastocysts, which differentiated into mature and functional parathyroid glands within the chimeric mouse body.
Yes, the transplanted mESC-derived parathyroid glands showed promising results in improving the pathology of a hypoparathyroidism model mouse. This outcome suggests that regenerating and transplanting functional PTGs could offer a potential new treatment option for hypoparathyroidism in the future.
Yes, the study demonstrated success in cross-species studies as well. The researchers were able to produce functional mouse parathyroid glands in rats using the same blastocyst complementation method. This opens up possibilities for potential applications in various species, including humans.
While the study was conducted in mice and rats as a first step, it lays the groundwork for potential clinical applications in the future. Before applying the method to humans, further research and testing will be necessary to ensure its safety and efficacy.
More information: Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2216564120